ART for head and neck cancer
The effects of anatomical changes and variation in daily patient set-up on the quality of proton plans for head and neck cancer
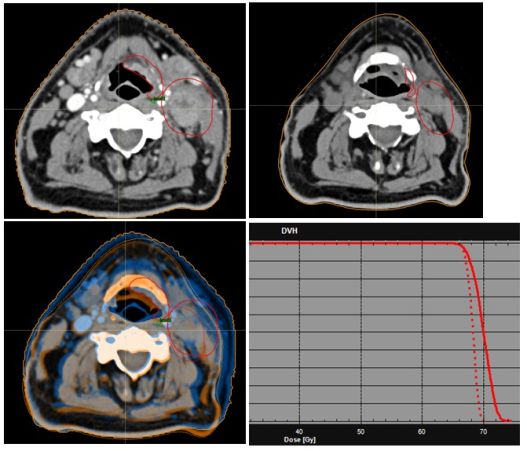
A radiotherapy course for head and neck cancer involves daily radiation treatments over a period of up to seven weeks. The patient must be positioned with high precision, allowing only small variations from day-to-day, in order to reproduce the desired dose distribution of the treatment plan. Despite patient-specific immobilization devices and online image guidance, patient positioning in the head and neck area can be problematic. The patient anatomy may also change during the treatment course, for example due to; weight loss, swelling, variation in the tumour size or shape, and filling of sinuses. If these deviations are not taken into account accurately, they may lead to errors in the dose delivery because of the physics properties of proton beams.
Despite a large variation in anatomy, adequate target coverage was maintained during the treatment course without plan adaptation
We are investigating several mitigation strategies, including the benefit of a-priori robust optimization (where the treatment plan is derived taking into account certain simulated errors), different beam configurations, and the use of beam-specific target volumes and avoidance structures. This research is based on repeat CT-imaging data of patients from our photon clinic.
The ultimate aim of the study is to strike a balance between the need to have robust target coverage throughout the treatment course, and maintaining an NTCP advantage over photon therapy, whilst minimizing the frequency of plan adaptations. A further outcome would be to determine which patient groups are more likely to require plan adaptations and to perhaps tailor mitigation strategies prior to treatment.
People involved
Dan Scandurra, Martijn Gelderman, Roel Kierkels, Henk Bijl, Hans Langendijk.
Geometric and dosimetric variability in head and neck organs at risk during the course of treatment
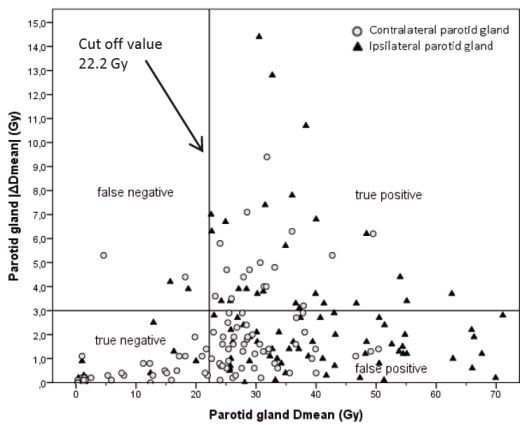
During the course of treatment of a head and neck tumor, anatomical changes in the organs at risk (OARs) may lead to dosimetric compromises. We provide an overview of the magnitude and frequency of these effects, and investigate criteria to identify head and neck cancer patients who may benefit from adaptive radiotherapy (ART).
Potential pre-treatment selection criteria identified are the tumor location (nasopharyngeal carcinoma), age, body mass index, planned dose to the parotid glands, the initial parotid gland volume, and the overlap volume of the parotid glands with the target volume. These criteria will be further extended for photon and proton therapy, and several adaptive treatment strategies will be explored. One of our current interests is to include image biomarkers for determining the best adaptive treatment strategy.
In the figure above, deviations from the planned parotid gland mean dose (|ΔDmean|) are shown on the y-axis. Selection of patients for |ΔDmean| > 3 Gy with 91% sensitivity could be performed by using the threshold of 22.2 Gy for the dose to the parotid gland.
People involved
Charlotte Brouwer, Marianna Sijtsema, Roel Steenbakkers, Sanne van Dijk, Tian-Tian Zhai, Hans Langendijk.
References
C.L. Brouwer et al. Selection of head and neck cancer patients for adaptive radiotherapy to decrease xerostomia. Radiother Oncol 2016 122(2):185-191 (pdf)
C.L. Brouwer et al. Identifying patients who may benefit from adaptive radiotherapy. Radiother Oncol 2015 115(3):285-94 (pdf)
Dijk LV Van, Brouwer CL, van der Laan, et al: Geometric Image Biomarker Changes of the Parotid Gland Are Associated With Late Xerostomia. Int J Radiat Oncol Biol Phys 2017 99(5):1101-1110 (pdf)

 English
English
 Nederlands
Nederlands