NTCP-based treatment planning optimization
Project aim
Clinically validated multi-variable normal tissue complication probability models (NTCP) have recently become available for head and neck cancer (HNC) patients. We investigate the feasibility of using these models directly in the optimizer for inverse radiotherapy treatment planning, with the aim of improved dose distributions and corresponding NTCP-estimates in HNC patients.
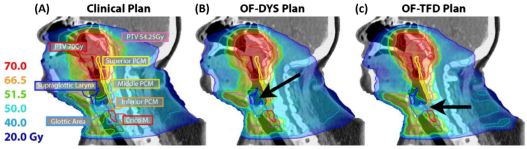
For >100 HNC cases, intensity-modulated radiotherapy (IMRT) plans were optimized using objective functions either based on the ‘generalised equivalent uniform dose’ (OFgEUD) or based on multivariable NTCP-models (OFNTCP). NTCP-models for patient-rated xerostomia, physician-rated RTOG grade II-IV dysphagia, tube-feeding dependence and various patient-rated aspects of swallowing dysfunction were incorporated. The NTCP-models included dose–volume parameters as well as clinical factors contributing to a personalized optimization process. The two optimization techniques were compared by means of ‘pseudo-Pareto fronts’ (target dose conformity vs. the sum of the NTCPs).
People involved
Roel Kierkels, Arjen van der Schaaf, Erik Korevaar, Hans Langendijk.
Collaborators
Radiotherapeutisch Instituut Friesland, Netherlands:
Kees Schilstra
References
Kierkels et al. “Direct use of multivariable normal tissue complication probability models in treatment plan optimisation for individualised head and neck cancer radiotherapy produces clinically acceptable treatment plans” Radiotherapy and Oncology 112 (2014) 430-436 (pdf)
Kierkels et al. “Multivariable normal tissue complication probability model-based treatment plan optimization for grade 2–4 dysphagia and tube feeding dependence in head and neck radiotherapy” Radiotherapy and Oncology 221;3 (2016) 374-380 (pdf)

 English
English
 Nederlands
Nederlands